Limpopo Obstetric Response Team (LORT)
LORT is constituted of all categories of personnel within the health system that are directly and indirectly responsible for the health and wellbeing of pregnant women.
HOW IT STARTED
In implementing RMC in the pilot site and scaling it up to reach the entire province, the team provided training and on-site mentoring of healthcare workers and support staff. During this process, it was clear that the province needed clinical leadership and programme coordination, which was lost due to the disbanding of the District and Provincial Clinical Specialist teams. This was the determining factor in establishing the Limpopo Obstetric Team (LORT) in February 2020. LORT was established during the Joint Obstetric and Anaesthesia Symposium in February 2020 with the support of a Discovery Foundation grant awarded to the Department of Anaesthesiology via the then University of Limpopo Trust (ULT)t.
Categories of Personnel
LORT is constituted of all categories of personnel within the health system that are directly and indirectly responsible for the health and wellbeing of pregnant women, namely:
- Obstetricians
- Anaesthesiologists
- Midwives
- Emergency Medical Services (EMS)
- National Health Laboratory Service (NHLS)
- South Africa National Blood Service (SANBS)
- Pharmaceutical Depot
- Porters, Messengers
- Provincial & District Maternal Health Managers
- Development Partners
OUR GOAL
LORT’s ultimate goal is to eliminate all avoidable maternal deaths in the province through developing, adopting, and implementing innovative approaches and best practices. As a development partner, the ULT’s LimMCARE project tea, now Tree of Life Development Centre (ToLDC), supported LORT in rapidly assessing bottlenecks to improve the quality of obstetric/maternal care throughout the province. The bottlenecks identified included (and were corroborated by national research):
- Lack of adequate knowledge and skills amongst health care providers at PHC, district and regional hospitals
- Sub-optimal infrastructure, equipment, drugs and supplies at especially district hospitals, and a few regional hospitals,
- Absence of obstetric/maternal norms, standards and protocols for the province
- Sub-optimal to no implementation of RMC across the province
In 2023, ToLDC assisted LORT in securing funding from the private sector to contribute towards the Women’s Health Drive that took place in Thabazimbi from 14 -18 August 2023. The drive took place during the Waterberg Rural Matters campaign and saw over 60 healthcare providers (nurses and doctors) trained on safe caesarean sections, basic obstetric ultrasound, antenatal care, management of obstetric haemorrhage using the e-MOTIVE Helping Babies Breath and the Newborn Transition and Neonatal Resuscitation, interpreting pap smears and colposcopy as well as onsite mentoring on Respectful Maternity Care implementation. Get more details on the proceedings. The drive also included a community engagement event on the third day (16 August) led by the MEC of Health with community members, leaders, the private sector and businesses on improving maternal health. Services such as immunisation and health checks for chronic illnesses were provided. This event was also covered live by Thobela FM and Munghana Lonene FM, a feat made possible by donor funding. ToLDC provide onsite mentoring on RMC in addition to the coordinating support. This included international and nationally renowned specialists such as Dr Verenga from the University of Zimbabwe, Prof Sue Fawcus, an Emeritus professor from University of Cape Town (UCT), Prof Matsela from SMU, as well as Prof Maswime and Dr Moloi from UCT’s Global Surgery.
SUPPORT
This is the continuation of team’s support to LORT, that was provided under the University of Limpopo Trust, and this include the following:
1. The launch of the Limpopo Obstetrics and Gynaecology Protocols and Standards
The team supported the Department of Obstetrics and Gynaecology in developing and launching the first-ever Limpopo Obstetrics and Gynaecology Protocols and Standards. This work started in 2021 with a small team led by the Head of the Clinical Department, Dr Kaizer Baloyi, who led the drafting of the protocols, followed by two consultative workshops to get feedback from the rest of the LORT team members. The protocols were finally finalised and approved. The team decided to have a launch for better dissemination to the entire province
The launch was held on 28 October 2022 in Polokwane during the Rural Health Matters campaign in Capricorn District. This meant that over 60 healthcare providers who were participating in the Obstetrics and Neonatal training drive were able to attend the launch. The booklet covers obstetric and gynaecology protocols, anaesthesia protocols and guidelines, the updated Limpopo Maternal Health Standards and the RMC SOP. This was necessitated by healthcare providers using protocols from the institutions where they were trained. This posed a challenge where as much as the basic principles of obstetrics remain the same across various training institutions, their protocols are primarily tailored for the health systems in which the training institutions are located (e.g. KwaZulu-Natal, Western Cape, Gauteng) and not for Limpopo.
2. Women’s Health Drive in 2022
The Women’s Health Drive in 2022 occurred on August 18 – 22 during the Rural Health Matters Campaign in Waterberg district. The Women’s Health Drive was based in Polokwane, and it aimed to reduce the surgical backlogs for urogynaecology and urology. The target was to operate on 26 patients from rural communities and transfer skills to about 50 specialists from the province from the leading team of surgical experts. The surgical team included our champion Dr Muavha, Dr Masegela, a urologist and Head of Clinical Unit: Urology at Pietersburg Hospital, Prof Kruger, a urogynaecologist from Alberta University in Canada, Dr Moshokoa, a urologist (first black female in SA) in the private sector, Dr Brouard, a urogynaecologist from UCT/Groote Schuur Hospital, Dr Ndhlovu a reproductive medicine specialist in the private sector, Dr Blaauwhof a gynaecologist in the private sector.
3. Virtual Provincial Obstetrics Symposium in 2020
This was the first and most successful virtual symposium series focused on key topics of the international Essential Steps in the Management of Obstetrics Emergencies (ESMOE) and Basic Ultrasound training programmes. The virtual symposium ran 6 weeks (09 September – 04 December 2020), included national and international facilitators, and reached a national and Southern African Development Community (SADC) region audience. The sessions from the symposium were recorded and made accessible to healthcare providers who could not attend the live sessions. The symposium reached a minimum of 4723 health care professionals from all 9 provinces in SA and other African countries, i.e., Zimbabwe, Malawi, Namibia, Botswana and Ghana. This is because the official numbers are unique logins, and there were facilities, especially in Limpopo, where a team in a facility or ward logged in with one computer.
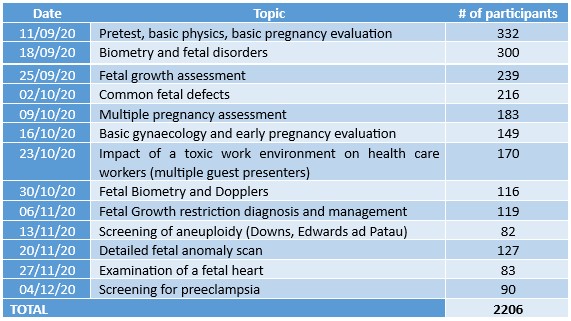
Breakdown of basic ultrasound course participants by topic presented by Dr Verenga from the University of Zimbabwe
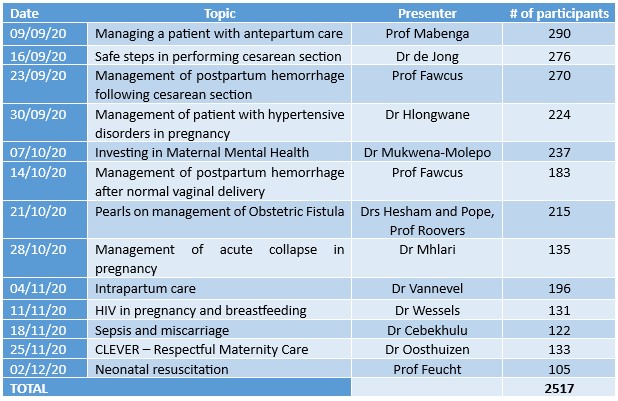
Breakdown of ESMOE course participation by topic
4. Other Clinical Mentoring and Support
A Discovery Foundation grant through the ULT for Prof Sue Fawcus and Emeritus Professor at UCT and a key member of the National Committee for Confidential Enquiries into Maternal Deaths (NCCEMD), be a distinguished visitor from 2020 to 2022 to provide clinical mentoring and support. Her critical support by her support during the Joint Obstetrics and Anaesthesia Symposium in 2020 where she gave practical training on how to use the Non-pneumatic Anti-shock Garment (NASG) to manage postpartum haemorrhage (PPH) to over 100 healthcare providers who attended the symposium (see pictures below). The NASG is a first‐aid device that can stabilise women in hypovolemic shock secondary due to PPH until the patient can obtain definitive treatment. Lightweight and reusable, the NASG is made of neoprene and Velcro with a small foam ball to provide uterine compression. The device has five neoprene segments that wrap tightly with Velcro around the legs, pelvis and abdomen in that order if applied correctly. The NASG, however, is not a cure for PPH but is considered a part of the resuscitation measures to help control the source of bleeding.
Prof Fawcus giving a lecture and demonstrating the use of NASG with participants in 2020





Prof Fawcus also provided periodic in-person and virtual mentorship visits to support LORT in improving their clinical leadership in addressing critical bottlenecks in providing quality obstetrics and maternal health services throughout the health system. These include:
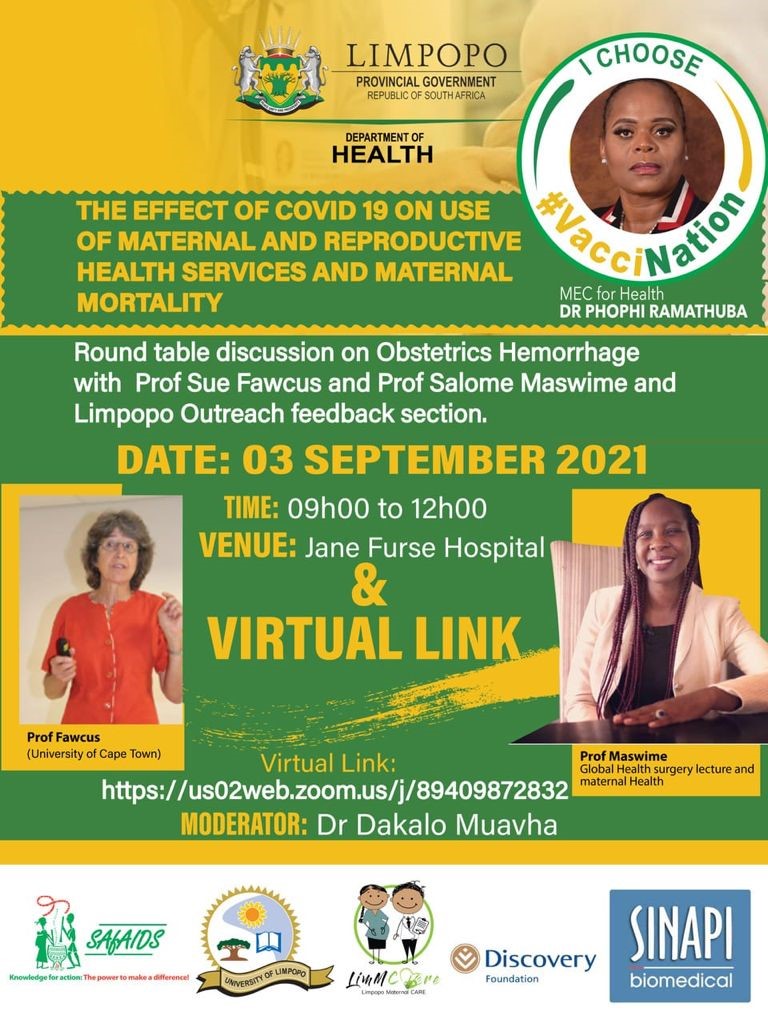
Prof Fawcus’ site visit 30 August – 03 September 2021
Prof Fawcus visited the province at the backdrop of a three-week support of three Limpopo hospitals by three newly qualified specialist obstetricians from the UCT. The team was organised by Profs Fawcus and the support costs were funded by SAfAIDS. During her visit, she visited 9 hospitals (Malamulele, Nkhensani, Helen Franz, Jane Furse, and Dilokong, Elim and Donald Fraser [district hospitals], and Letaba [regional hospital] and Pietersburg [tertiary hospital]). She was accompanied by Dr Kaizer Baloyi (provincial Head of O&G, Dr Dakalo Muavha (urogynae specialist at Pietersburg hospital and co-coordinator of the LORT and Prof Salome Maswime, Head of Global Surgery at UCT) on all days and Dr Nyatozi Chirwa (specialist at Pietersburg hospital) for two days. The purpose of the visit was to review the impact of LORT and the placing of the three specialists at the district hospitals and assess the successes and challenges around maternal health care in the hospitals visited. The Chief Executive Officers (CEOs), Clinical managers, maternity doctors and midwives participated in the visits and hospital walk abouts.
From this visit, Prof Fawcus shared improvement recommendations, which were both immediate and long-term. Immediate recommendations included the finalisation and dissemination of protocols for clear guidance on managing patients on the ground and the commencement of outreach from Regional and Tertiary hospitals to cover all District hospitals to maintain the momentum started by deploying the O&G specialists. Other recommendations were specific to the key issues at the hospitals visited and the appointment of specialists at Letaba and St Rita’s, the two regional hospitals without specialists in the province.
Three weeks support form 3 UCT obstetricians (16 Aug – 03 September 2021) and a Virtual Obstetrics Symposium on 03 September 2021
The team from UCT consisted of newly specialised obstetricians and they supported Limpopo for three weeks. They were based at three district hospitals (Malamulele, Helen Frans and Jane Furse with outreach to Nkhensani, and Dilokong). The main aim of the visits was upskilling doctors and midwives in maternal health, and ensure competency in assisted delivery and caesarean section (CS). The three specialists were to conduct bed-side/hands-on mentoring during consultation and surgical cases as well as training on key topics.
During the visits, there was a weekly virtual feedback session to share learnings from each specialist and their hosting facility. The rest of the facilities in Limpopo were also urged to join these session as they were available for all in the province. From the experiences and assessments of the three specialists, it was clear that they have overcome some of the challenges faced by the individual hospitals in which they were placed, they had consolidated CS skills, introduced skills for assisted deliveries (vacuums) which were previously not being performed, conducted training and drills with doctors and midwives and provided much appreciated support and supervision to MOs and COSMOs working in maternity.
At the end of the visit, the team organised a symposium at Jane Furse Hospital as a consolidation and feedback of the support. The session was also virtual to allow for all hospitals to attend the session. Prof Fawcus presented the current evidence-based protocols for PPH after CS and Prof Maswime presented an overview of the UCT’s Global Surgery objectives and its link to improving quality care as part of final feedback session for the support (see official poster for the session on the right). During the session, it was clear from the hosting hospital management that the team has made enormous difference in the three weeks that they were in Limpopo.
PPH symposium 21 July 2022
The team organised a PPH symposium in the backdrop of the 5-day Ellavi uterine balloon tamponade (UBT) training roadshow in Limpopo. The aim of the symposium was to educate healthcare workers in Limpopo about algorithms for the management of PPH (presented by Prof Fawcus) as well as discuss the use of the Ellavi UBT in the management of PPH (presented by Prof. Gerhard Theron from Ellavi). The symposium was a combination of virtual and in person, where people from all facilities in Limpopo joined as well as from the rest of South Africa and in other African countries (Ghana, Uganda and Kenya teams as part of the panellists). From Limpopo, the symposium reached over 50 people in person, who comprised of representatives from the tertiary, regional and district hospitals as well as provincial and district maternal health managers. A more emphasis was placed on representatives from Capricorn district. The team that attended the session in person also had an opportunity of having a practical session on Inserting, monitoring & removing the Ellavi UBT. This was due to the fact that the symposium was partly a training session for the Capricorn district team.